NHS deficits hit 'massive' £930m
- 9 October 2015
- Health
 Thinkstock
Thinkstock
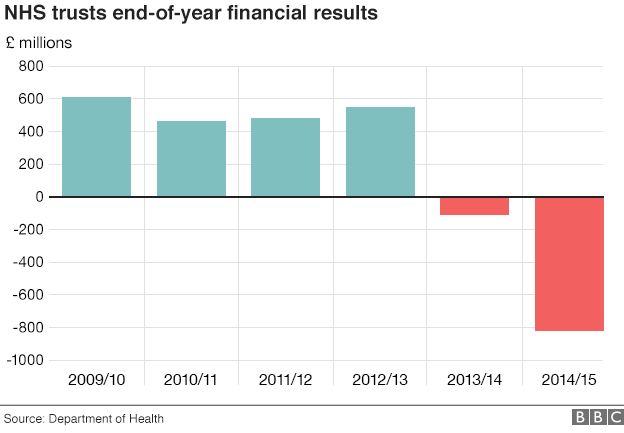
NHS trusts in England have racked up a £930m deficit in the first three months of the financial year - that is more than the entire overspend last year.
Regulators said the problems were the "worst for a generation" and demanded immediate action be taken.
The scale of the deficits - eight in 10 trusts are in the red - also prompted warnings that care would suffer.
The accounts cover hospital, mental health, ambulance and some community services.
Between them they account for about two-thirds of the NHS's £116bn budget - with the rest going on other areas including GPs, drug prescribing and training.
Last year, NHS trusts overspent by £822m - with the health service as a whole balancing the books only after a cash injection from the Treasury and by raiding the capital budget earmarked for buildings.
NHS deficit
£930m
NHS trusts deficit for April to June 2015
- £451m deficit for same period last year
- £822m total overspend for the whole of last year
- £2bn estimated deficit for the 2015/16 financial year
But it is thought unlikely there will be the money in the system to plug the shortfall if the financial situation continues to deteriorate in this way.
It has been suggested the deficit among the 237 NHS trusts could top £2bn this year.
The figures released by the two regulators - Monitor and the Trust Development Authority - show the NHS is on track for that as spending pressures do tend to ease as the financial year goes on.
Nonetheless, trusts - and in particular hospitals - are now under pressure from regulators to make savings.
Spending on agency staff has been highlighted as one of the biggest potential savings, but the accounts also show that rising demands year-on-year have been gradually making it harder for trust to break even.
David Bennett, chief executive of Monitor, said: "Today figures reiterate the sector is under massive pressure and must change to counter it.
"The NHS simply can no longer afford operationally and financially to operate in the way it has been and must act now to deliver the substantial efficiency gains required."
However, most experts believe the NHS has little wriggle room to improve its performance.
Chancellor George Osborne said: "More than £2bn extra are going into our health service this year with more to come.
"Clearly the NHS has to spend that money well and deal with things like rip-off nursing agencies and management consultancies that charge too much.
"We want the money going to the frontline."
'Challenging'
Nigel Edwards, chief executive of the Nuffield Trust think-tank, said: "Financial problems on this scale cannot be explained by individual pockets of mismanagement - we are looking at a systematic problem across the health service.
"It is becoming increasingly impossible to provide quality standards, timely access to care and financial control at the same time."
Paul Healy, from the NHS Confederation, which represents trusts, said: "Hospitals and other front-line organisations have all-but exhausted their options for becoming more efficient."
He said it was important that the extra money being promised to the NHS this Parliament was front-loaded so that most of it came in the first few years.
But the Department of Health said there were still savings that could be made - and it expected performance would improve as the year goes on.
Analysis: Do deficits matter?
It is easy to be blase about NHS deficits and think the money will always be found to bail out the health service. That is the case - but only to a certain extent.
While there are a number of trusts that have been overspending for years and have been kept afloat by the wider system, the support is not endless.
Three years ago, South London Healthcare, which ran three hospitals, was allowed to go under after racking up large deficits.
Howhe problem this year goes beyond individual NHS trusts and to the very heart of government.
A deficit on the scale of £2bn among trusts will make it incredibly difficult for the Department of Health to balance the books overall.
If that happens, it will have to go cap in hand to the Treasury. For a service that is being protected from cuts to have to do this raises some very difficult questions all round.
Alongside the financial data, the regulators have also warned about worsening waiting times for hospital treatment.
Latest figures show:
- The number waiting for non-emergency operations, such as knee and hip replacements, is 3.3 million - the highest level since early 2008
- The 62-day cancer waiting time target has been missed for the past 16 months
- The four-hour A&E target has been missed for 11 of the past 12 months
Newcastle upon Tyne Hospitals NHS Foundation Trust chief executive Sir Len Fenwick, the longest-serving hospitals boss in the health service, told the BBC the pressures were likely to mean winter would be extremely difficult.
He predicted non-emergency operations would need to be delayed to help hospitals cope.
"In the coming winter, we do believe there will be greater pressures than ever before," he added.
ever, t